Ectopic pregnancy
Ectopic pregnancy is a complication of pregnancy in which the embryo attaches outside the uterus. Signs and symptoms classically include abdominal pain and vaginal bleeding. Fewer than 50 per cent of affected women have both of these symptoms. The pain may be described as sharp, dull, or crampy. Pain may also spread to the shoulder if bleeding into the abdomen has occurred. Severe bleeding may result in a fast heart rate, fainting, or shock. With very rare exceptions the fetus is unable to survive.
Risks Factors Include
- The pelvic inflammatory disease often due to chlamydia infection
- Tobacco smoking
- Prior tubal surgery
- History of infertility
- Use of assisted reproductive technology
Those who have previously had an ectopic pregnancy are at much higher risk of having another one.
Detection
Detection of ectopic pregnancy is typically by blood tests for
- Human Chorionic Gonadotropin
- Ultrasound
Complications
The most common complication is a rupture with internal bleeding which may lead to
hypovolemic shock. Death from rupture is the leading cause of death in the
first trimester of the pregnancy.
Diagnosis
Ectopic pregnancy should be considered as the cause of abdominal pain or vaginal bleeding in every woman who has a positive pregnancy test. The primary goal of diagnostic procedures in possible ectopic pregnancy is to triage according to risk rather than establishing pregnancy location.
Transvaginal ultrasonography
Other methods
- Direct examination
A laparoscopy or laparotomy can also be performed to visually confirm an ectopic pregnancy. This is generally reserved for women presenting with signs of an acute abdomen and hypovolemic shock.
- Culdocentesis
- Progesterone levels
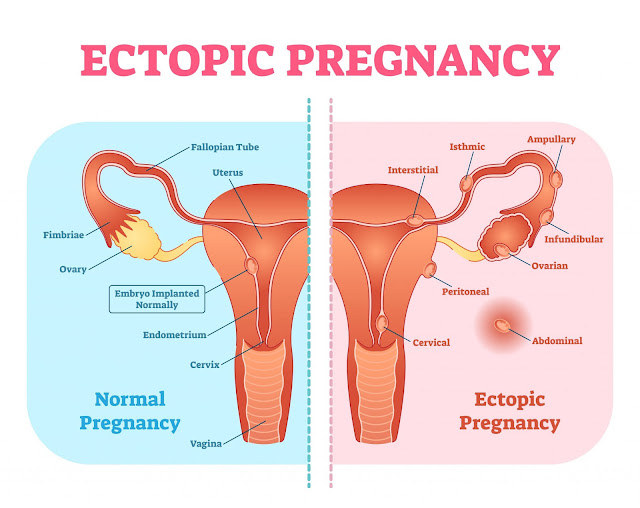
Classification
a) Tubal pregnancy
The vast majority of ectopic pregnancies implant in the Fallopian tube. Pregnancies can grow in the fimbrial end (5% of all ectopic pregnancies), the ampullary section (80%), the isthmus (12%), and the cornual and interstitial part of the tube (2%).
b) Nontubal ectopic pregnancy
Two per cent of ectopic pregnancies occur in the ovary, cervix, or are intra-abdominal. Transvaginal ultrasound examination is usually able to detect a cervical pregnancy.
c) Heterotopic pregnancy
In rare cases of ectopic pregnancy, there may be two fertilized eggs, one outside the uterus and the other inside. This is called a heterotopic pregnancy.
d) Persistent ectopic pregnancy
A persistent ectopic pregnancy refers to the continuation of trophoblastic growth after a surgical intervention to remove an ectopic pregnancy. After a conservative procedure that attempts to preserve the affected fallopian tube such as a salpingotomy, in about 15–20% the major portion of the ectopic growth may have been removed, but some trophoblastic tissue, perhaps deeply embedded, has escaped removal and continues to grow, generating a new rise in hCG levels. After weeks this may lead to new clinical symptoms including bleeding. For this reason, hCG levels may have to be monitored after removal of an ectopic pregnancy to assure their decline, also methotrexate can be given at the time of surgery prophylactically.
e) Pregnancy of unknown location
Pregnancy of unknown location (PUL) is the term used for a pregnancy where there is a positive pregnancy test but no pregnancy has been visualized using transvaginal ultrasonography. Specialized early pregnancy departments have estimated that between 8% and 10% of women attending for an ultrasound assessment in early pregnancy will be classified as having a PUL.




Comments
Post a Comment